3.1 Understanding brain death
What is brain death?
Brain death is when all blood flow to the brain has irreversibly ceased and the whole brain has died. The patient is apnoeic. Ventilation and circulation are mechanically supported which allows function of other organs to continue. Brain death is death that is diagnosed using neurological criteria.
How brain death occurs
Brain death occurs when severe brain damage leads to marked elevation of intracranial pressure. When intracranial pressure reaches systemic blood pressure, intracranial blood flow stops and the whole brain, including the brainstem, dies.
How brain death is determined
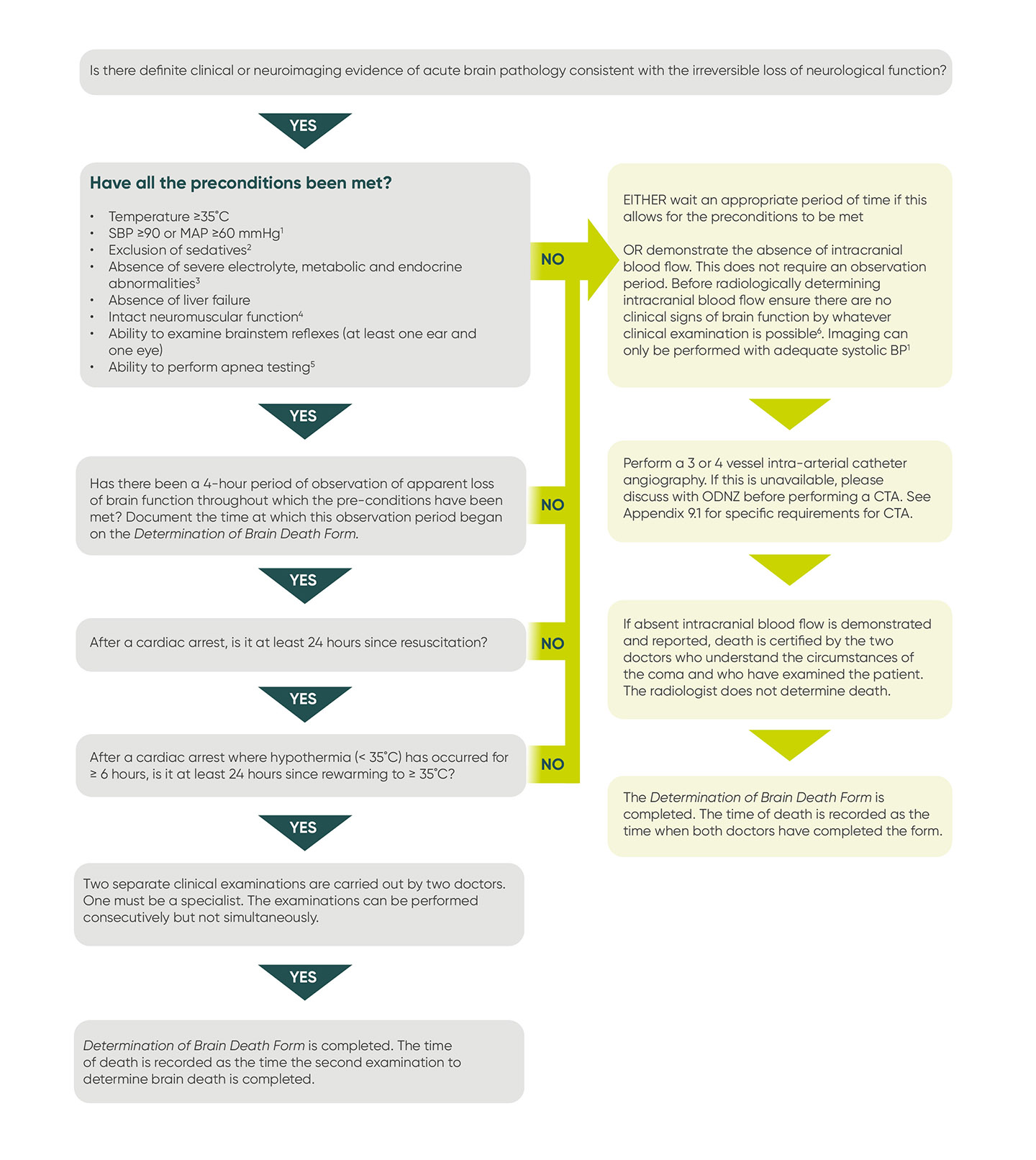
ODNZ requires the determination of brain death to be in accordance with the standards defined in the ANZICS Statement. For details of preconditions, observation periods, clinical examination, alternatives to clinical examination, and determination of brain death in infants and children, see Section 3.2.
Who can determine brain death?
The ANZICS Statement specifies that:
”Neurological determination of death is carried out by two doctors, one of whom should be a specialist, who must each independently determine death according to this Statement, and meet the requirements of jurisdictional legislation.”
There is no legislative requirement in New Zealand. ODNZ requires that at least one of the two doctors must be a specialist.
Brain death testing in children
The ANZICS Statement specifies that:
“The criteria for neurological determination of death in children above the age of 30 days are the same as those in adults.”
The criteria for neurological determination of death in neonates below the age of 30 days are covered in the ANZICS Statement. Consultation with ODNZ is recommended in these circumstances.
Family observation of clinical brain death testing
ODNZ recommends that families are offered the opportunity to observe the clinical examination. The family should be told:
- what brain death is
- how it is determined
- who will do the examination(s)
- that spinal reflexes may occur
- that a staff member will be present to support them.
This should be in sensitive non-medical language.
The family may not wish to observe the examination and this decision must be respected. However, for those who are uncertain about observing, there is evidence that this can improve their understanding of brain death without increasing their distress.
Some family members wish to be present at the time of death. This is at the end of the second clinical examination.
Before each examination, the doctor responsible should ensure that any family members present have received an explanation of what they are going to see.
Here is an example:
"We suspect that the blood flow to (name’s) brain has stopped and that his/her brain has died. In order to confirm this, two doctors will both carry out a very specific examination. This involves examining to see if (name’s) brain responds to stimulation, including pain, and if he/she can breathe.
Sometimes there can be movements that come from the spinal cord and not the brain, for example movement of an arm or leg. If this happens, I will explain this to you.
If you want to be there when the examination is carried out, (name of staff member) will be there to support you and answer any questions.”
Explaining determination of brain death by imaging to the family
Here is an example:
“We suspect that the blood flow to (name’s) brain has stopped and that his/her brain has died. In order to confirm this, he/she will have a special scan to see if there is any blood flow to his/her brain.”
Explaining brain death to family members
Here is an example:
“(Name’s) brain has swollen because of (insert specific diagnostic reasons). The pressure inside (name’s) skull has become so high it has cut off the blood supply to his/her brain. As a result, his/her brain has died and I’m sorry, this means that (name) has died.”
Be prepared to explain about how mechanical ventilation allows the heart to continue to beat and for the skin to be pink and warm.
3.2 Determining brain death
Hypothermia and determining brain death
The reference to hypothermia is only in the context of hypoxic ischaemic encephalopathy (HIE). This is most likely to be following a cardiac arrest but also possibly a respiratory arrest. The hypothermia will directly affect brain function and therefore a 24-hour observation period at temperature of more than 35°C must be observed prior to brain death testing. The last 4 hours of this 24-hour period can be counted as the 4-hour observation period “of GCS 3 with pupils non-reactive to light, absent cough/ tracheal reflex and apparent apnoea on a ventilator”.
In the case of hypothermia <35 °C for more than 6 hours in non-HIE brain injury (eg meningitis, OD, stroke, ICH) where there is apparent loss of brainstem reflexes, the period before testing is determined by whether hypothermia may have altered drug metabolism. The type and amount of drug and its clearance under hypothermia conditions will need to be considered. Discussion with the ODNZ on call medical specialist is encouraged.
3.3 Observations compatible and incompatible with brain death
There are a number of observations which are sometimes found in patients with deep coma, some are compatible with brain death and must be distinguished from those that are not compatible with brain death. Some of these observations can occur during clinical examination. It is important to be able to explain these observations and their significance to healthcare workers and to family members who might observe them at the bedside or during clinical examination.
Observations compatible with brain death
- Spinal reflexes
- Sweating, blushing or tachycardia
- Normal blood pressure without the need for pharmacological support
- Absence of diabetes insipidus (DI)
- Having an ICP<MAP
Spinal reflexes
Spinal reflexes do not occur in the motor distribution of the cranial nerves or in response to stimulation within the cranial nerve distribution.
Spinal reflexes can be either spontaneous or elicited by stimulation, such as:
- a painful stimulus applied to limbs or sternum
- tactile stimulation applied to palmar or plantar areas
- neck flexion
- limb elevation
- hypoxia during ventilation disconnection.
Spinal reflexes should not be confused with abnormal flexor or extensor responses.
It should be explained to family members that spinal reflexes involve only the spinal cord, not the brain. Spinal reflexes should be explained to healthcare workers as occurring as a result of connections within the spinal cord between an afferent (sensory) limb and an efferent (motor) limb of a spinal reflex.
Spinal reflexes may include:
- extension-pronation movements of the upper limbs
- undulating toe reflex (plantar flexion of the great toe, followed by brief plantar flexion sequentially of second to fifth toes)
- Lazarus sign (bilateral arm flexion, shoulder adduction, hand raising to above the chest, and may include flexion of trunk, hips and knees)
- deep tendon reflexes
- plantar responses (either flexor or extensor)
- respiratory-like movements (shoulder elevation and adduction, back arching or intercostal expansion) without significant tidal volume
- head turning.
ODNZ can help with identification of these movements. If there is any doubt as to the origin of the movement, a cerebral blood flow study must be performed.
Observations incompatible with brain death
- Decerebrate or decorticate posturing
- True extensor or flexor motor responses to painful stimuli
- Seizures
- Limb movement elicited by stimulation in the cranial nerve distribution
- Facial movement elicited by stimulation in the torso/limbs
3.4 Sequence of events in DBD
The patient has devastating brain damage which is likely to be fatal and is on a ventilator.
↓
ODNZ is contacted to discuss the potential for organ and tissue donation.
↓
The ICU Link nurse is contacted in some hospitals.
↓
Blood is taken for the Donor Blood Pack and the ODNZ donor coordinator arranges transport.
↓
Brain death is determined and documented.
↓
Donation is discussed with the family.
↓
The agreement of the coroner is obtained when required. The coroner must consider the family’s views regarding donation.
↓
Donor information is obtained and required documentation is completed.
↓
Donor coordinator organises the organ donation.
↓
Organ donor surgery.
↓
Family may wish to spend time with their relative.
3.5 Checklist for donation after brain death (DBD)
Please contact the donor coordinator to discuss any aspect of the donation process.
In this document the term intensivist refers to a senior doctor (specialist or fellow) looking after the patient. In some hospitals this might be an anaesthetist or other specialist. The term any doctor is used when actions do not require a senior doctor to be involved. ICU staff is used when actions could be done by an ICU doctor or ICU nurse.
These procedures for organ donation after brain death are listed in approximate sequence.
|
TASK |
ACTION BY |
ACTION |
|
1. Identify the possibility of donation |
ICU staff |
Please call the donor coordinator to discuss any patient with severe brain damage who is likely to die (09 630 0935). |
|
2. Initial assessment |
Donor coordinator/ ODNZ medical specialist |
The donor coordinator:
|
|
3. Notify ICU Link Nurse |
ICU staff |
In most hospitals the ICU staff ask the ICU Link nurse to assist. |
|
4. Take blood for the Donor Blood Pack |
ICU staff |
The labels on the ABO blood tube (pink tube) must be hand-written. Patient labels can be used on all other blood tubes and the laboratory blood form (enclosed in the Donor Blood Pack). Check blood tubes are not out of date. |
|
5. Transport of the Donor Blood Pack |
Donor coordinator |
The donor coordinator arranges transport of the Donor Blood Pack from the ICU to Auckland. This is done as soon as possible to prevent undue delays for the donor family if donation does go ahead. Blood is only tested after the family has agreed to donation. |
|
6. Inform family |
Intensivist and ICU nurse |
The family is informed that brain death is likely to have occurred and that this will be determined by either clinical examination or by demonstration of absent blood flow to the brain. |
|
7. Determination of brain death |
Two doctors including at least one specialist |
Brain death is determined either by clinical examination or by demonstration of absent cerebral perfusion. In either case there must be evidence of intracranial pathology consistent with the irreversible loss of neurological function. See the ANZICS Statement for details of the clinical examination. See Section 9.1 for the details of demonstration of absent cerebral perfusion. |
|
8. Documentation of brain death |
Two doctors including at least one specialist |
Brain death is documented on the Determination of Brain Death Form. When brain death has been determined by clinical examination, the time of death is recorded as the time when the second clinical examination to determine brain death is completed. When brain death has been determined on the basis of absent cerebral perfusion, the time of death is recorded as the time when the two doctors have completed the Determination of Brain Death Form. |
|
9. Inform family |
Intensivist and ICU nurse |
The intensivist informs the family that the patient is brain dead and of the time of death. The ICU nurse is present at this family meeting. |
|
10. Discussion of donation with the family |
Intensivist and ICU nurse |
The intensivist discusses donation with the family. The ICU nurse and sometimes an ICU Link nurse is also present at this family meeting. |
|
11. Discussion with the coroner |
Intensivist |
The Coroners Act 2006 defines the circumstances where a death must be referred to the coroner. The coroner may or may not “accept jurisdiction”. In cases where the coroner accepts jurisdiction, the removal of organs and tissues cannot proceed without the agreement of the coroner. The intensivist discusses organ and tissue donation with the coroner. The coroner must be informed of the family’s views about donation as the coroner is required to consider these views. The coroner has agreed to donation in some cases of suspected homicide. See Section 8.3. |
|
12. Refer back to donor coordinator |
ICU staff |
The ICU staff inform the donor coordinator of the outcome of the family discussion. If the family agrees to donation, the donor coordinator requests all the necessary details for donation. See Section 8.4 |
|
13. Routine death documentation |
ICU doctor and nurse |
Routine death documentation is completed in accord with local hospital practice and kept with the clinical notes. |
|
14. Identification of the deceased |
Any ICU doctor or nurse |
Where the coroner has taken jurisdiction, the ICU medical staff notify the police before the donor surgery. The ICU staff may need to explain brain death to the police. Showing the Determination of Brain Death Form may assist in understanding that death has occurred. The police will require the family to identify the deceased patient. The ICU staff should try to ensure this is done before the family leaves the hospital and prior to the donor surgery. This is to avoid the family having to return to the hospital. |
|
15. Medical/Social Questionnaire and Physical Assessment Form completed |
ICU staff or donor coordinator |
The ICU staff or donor coordinator completes the Medical/ Social Questionnaire for Organ and Tissue Donation with a family member(s) and the Physical Assessment Form. |
|
16. Liaison with transplant teams |
Donor coordinator |
The donor coordinator liaises with the transplant teams and tissue banks to determine which organs and tissues can be donated for transplantation. |
|
17. Notification of ICU staff of any organ and tissues accepted |
Donor coordinator |
The donor coordinator informs the ICU staff which organs and tissues can be donated for transplantation and any requests for tissues for specific research projects. |
|
18. Authority for organ and tissue removal |
ICU staff |
ICU staff inform the family which organs and tissues can be donated for transplantation and any requests for tissues for specific research projects. A family representative signs the Authority for Organ and Tissue Removal Form or witnessed verbal consent is obtained. The ICU staff notify the donor coordinator of the outcome of this process. |
|
19. Completion of documentation |
Donor coordinator and ICU staff |
The donor coordinator ensures that completed forms have all been received from the ICU: The Medical/Social Questionnaire must not to be left in the patient notes. The donor coordinator will take the original when they arrive at the donor hospital. |
|
20. Organisation of the donor surgery |
Donor coordinator |
The donor coordinator liaises with the ICU, OT, anaesthetist (if needed) and the transplant team(s) to arrange the time for the donor surgery. The donor coordinator informs the ICU and OT staff which organs and tissues have been accepted for donation. |
|
21. Crossmatching |
ICU staff |
ICU staff crossmatch 4 units of RBC for the donor surgery. |
|
22. Medical treatment of the donor in ICU |
ICU staff/ODNZ |
The ICU staff continue medical treatments to support extra- cranial physiology until the patient is transferred to the OT (see Section 4). They should notify the donor coordinator or the ODNZ medical specialist of any deterioration. |
|
23. Meet the family |
Donor coordinator |
Unless the family does not want to meet, the donor coordinator meets with the family, answers any questions, offers handprints and locks of hair, determines any requests following the donor surgery and what follow-up the family wishes to receive. |
|
24. Medical treatment of the donor in OT |
Anaesthetist |
An anaesthetist transfers the patient from ICU to OT and continues medical treatment until aortic cross clamp. ODNZ recommends the use of both neuromuscular blockade and measures to control sympathetic cardiovascular responses during donor surgery. See section 4.7. |
|
25. Time out in OT |
Donor surgeon |
The donor coordinator ensures that a Time Out occurs. This includes introduction of all staff and checking of documentation. The Authority for Organ and Tissue Removal Form replaces the usual operation consent form. |
|
26. Care of the deceased patient |
Donor coordinator, OT nurses(s), ICU nurse |
Following the donor surgery, care of the deceased patient takes place in OT or ICU depending on hospital procedures. In some hospitals the OT is blessed after the donor surgery. The ICU nurse ensures that a suitable room is made available for the family if they wish to spend time with their family member after the donor surgery. In some hospitals, where the coroner has accepted jurisdiction over the death, the police transfer the deceased patient to the mortuary. |